A deadly bite: Why free medicine doesn't help against an epidemic claiming 3,000 lives in just one country every year

Thirteen-year-old Abhishek Nepali was bitten by a snake while sleeping at his grandmother’s home in Pyuthan, a hilly town in the Lumbini province of Nepal, some 250km west of capital Kathmandu, on June 5.
Though rushed to a nearby hospital within 10 minutes, the doctor on duty referred him to another facility without starting treatment, unaware of snakebite protocols. Abhishek died on the way.
This was not just a singular case of fatal snakebite in Nepal’s Terai region, the stretch of Nepal’s lowlands that lie south of the Himalayan foothills and that border India.
Madhav Acharya, 60, from a neighboring province, was bitten by a rattlesnake on the night of July 31, while he was sleeping. He was rushed to the medical college in Kohalpur and then referred to a hospital in Bheri, Lumbini province, one of the few that provides treatment for snakebite in the region.
He underwent treatment for 17 days and was intubated for 7 days. He survived, but the course of treatment cost him about 250,000 Nepalese rupees ($1886), a princely sum considering the average annual income is 200,000 Nepalese rupees ($1489), according to the IMF.
According to the Lancet, Nepal records 26,749 to 37,661 snake bites annually, leading to 2,386 to 3,225 deaths. The journal says most of the deaths are of women and children.
The UN’s World Health Organization (WHO) has added snakebite to the list of neglected tropical diseases, highlighting the need for stronger epidemiological evidence in endemic countries such as Nepal.
“Cases of snakebite have increased in Nepal from 2018-19,” Dr. Hemant Ojha, head of the zoonotic department of the Epidemiology and Disease Control Division in Nepal’s Ministry of Health and Population, told RT. The Lumbini region saw the maximum cases in 2021-22 while the Madhesh region and the Karnali region also saw a rise.
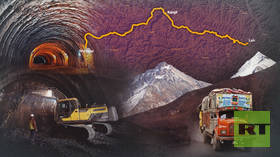
The Terai plains bordering India are most affected. A 2022 study found 37,661 cases and 3,225 deaths across 23 Terai districts each year. Snakes like cobras, kraits, and vipers are the biggest killers.
Govt calls snakebite ‘a disaster’
Nepal’s Home Ministry has listed snakebite as a disaster. The Nepalese Army operates snakebite treatment centers at 23 locations from Jhapa to Kanchanpur, spanning 18 districts, manned by 62 Army personnel supported by 19 health workers connected to local governments.
According to Health Ministry spokesperson Sameer Kumar Adhikari, Nepal has set a target of reducing the number of deaths due to snake bites by 50 percent by the year 2030, in line with the WHO’s stated goal of reducing snakebite incidents.
To achieve that goal, it is running programs such as raising awareness at the community level, training health workers, increasing the capacity of snakebite treatment centers and providing free anti-snake venom.
Keshab Shrestha, the mayor of Buddhabhumi Municipality in Kapilvastu district, is one elected representative who has taken a special interest in operating snakebite treatment centers and raising awareness on preventing snake bites.
Shrestha, who is serving a second term as mayor, told RT: ”To prevent death from snakebite, we have a treatment center in Gorusinghe with the help of the Nepal Army. We have arranged the necessary building, health workers, medicines, and ambulance for operating the center.”
Another poverty problem
A study in 2019-2020 by experts of the BP Koirala Institute of Health Sciences found that 40% of deaths due to snake bites occur in villages, another 40% die on the way to a hospital and about 20% die during treatment at hospitals.
Local authorities acknowledge that many additional incidents in remote villages go unreported, while the delay in reaching the hospital, lack of infrastructure, and belief in traditional healers instead of going straight to a hospital are also major reasons for snakebite fatalities.
A doctor based in Nepalganj’s state-run healthcare facility, told RT on condition of anonymity that ”Lack of awareness, poor healthcare infrastructure and expensive treatment trap victims in a vicious cycle.”
“In addition to private hospitals, government hospitals also treat snake bites,” he added. “The Ministry of Health procures close to 2,000 vials of ‘anti-snake venom’ from India every year and provides it free of cost to snakebite treatment centers and government hospitals.” However, he added,
”in practice, there is a major problem. Institutes do not have adequate stocks of anti-venom, there is a shortage of manpower as well as a lack of infrastructure. Also, the treatment is expensive for the poor.”
As a result, “people are forced to wait for death at home and depend on witchcraft,” said Dr. Chhabilal Thapa, author of ‘Medically Important Snakes and Snakebite Management in Nepal‘ said. ”The government needs to ensure adequate supply of anti-venom, train health workers in snakebite treatment and make it affordable for the masses.”
Though the government has declared snakebite treatment free, in reality ”victims have to bear heavy expenses for medicines, hospitalization etc,” he added. ”This forces them to opt for dangerous alternatives and leads to preventable deaths in many cases.”
Dr. Krishna Acharya, Senior Consultant Anesthesiologist at Bheri Hospital, Nepalgunj who treats snakebite victims, told RT that “it takes anywhere between 30 minutes to 10-12 hours for the venom to spread in the body, depending on the species of the poisonous snake.”
“Abdominal pain, vomiting, difficulty in breathing are the main symptoms,” he added. ”Patients with these symptoms should be rushed to a hospital or snakebite treatment center as soon as possible.”
“If a patient is taken to hospital within an hour of snakebite, the chances of saving her are over 90%,” Dr. Acharya said. ”That’s why doctors call the first hour after a bite the ‘golden hour’ for treatment.”
However, this is not the general practice in Nepalese society where there is a tendency to take the patient only after they become visibly weak, according to Dr. Acharya. As a result, most victims die on the way to a hospital.
No insurance coverage
According to data from the Ministry of Health for 2021-22, 926 people reached hospitals last year with snakebite. ”Treatment for such patients at hospitals costs at least one lakh [100,000] rupees,” Dr. Acharya said, adding, ”This is a very big amount for a family struggling to make ends meet. The government needs to make snakebite treatment completely free or provide financial support to poor families.”
The result is that though the government provides free anti-snake venom, patients have to pay out of pocket for other medicines, oxygen, ICU, ventilator, and the dialysis required for treatment. This should be provided free of cost or at highly subsidized rates to all snakebite victims, especially those from marginalized communities, Dr. Acharya believes.
“Around 40,000 families are directly affected every year, and close to 3,000 people die, which is a major public health issue in the country,” Dr. Acharya said. ”But the Ministry of Health, our political parties, and even the mass media have not given this adequate attention.”
He also felt local governments could help by providing free health insurance to residents of snakebite-prone areas. “If the insurance covers all expenses in case of a snakebite, it will reduce snakebite deaths and lessen the financial burden on families,” according to Dr. Acharya.
Dr. Thapa said information on what to do after a snakebite and where to take the patient for treatment has still not reached communities. Other than Kaligandaki Hospital in Nawalparasi, no other private hospital, clinic, or medical college in the district (in the southeast corner of Lumbini district, bordering India) treats patients bitten by snakes. Victims also do not get ambulances on time. People don’t even know which hospital is suitable for snakebite treatment.
Due to lack of facilities in the hospitals spread out in Terai’s districts (particularly those bordering India’s Terai), where the terrain is hilly and thus not easily accessible, patients bitten by snakes have to travel for hours.
Indian Forest Service officer J.P. Singh says in India’s Terai, venomous snakes like Russell’s Viper and the Indian Cobra find sanctuary in forested areas and their populations are regulated by natural predators like peacocks and other wildlife. In Nepal’s Terai, however, dwindling forest cover forces snakes into populated areas, leading to encounters with humans.
Abhishek, a Project Manager at the Nature Environment and Wildlife Society, has been working closely with snakes for over two decades. He says the surge in snakebite incidents in Nepal’s Terai can be attributed to heavy rains during monsoon. The rainfall displaces the snakes from Nepal’s hills, which then seek refuge in the low-lying Terai region, where rice cultivation creates a habitat rich in both snakes and their prey, including rodents. This leads to an increased likelihood of human-snake encounters.
As a result, patients from districts scattered in Lumbini province and in neighboring Sudurpaschim province, in Nepal’s southwest corner, have to go all the way to Bheri Hospital in Lumbini’s Nepalgunj for treatment. There are many instances of patients dying on the way due to not reaching a hospital on time
Taboo around menstruation also increases the risk of snakebites
In the second week of June, 15-year-old Hemanti Joshi from Sukhad, Kailali (in Sudurpaschim province) was bitten by a snake while sleeping on the porch during menstruation. She was taken to Seti Hospital Dhangadhi. She died a week after treatment.
There are also incidents of deaths of women and children from snakebites, while residing in the Chhaupadi (menstrual hut) in Nepal. In many parts of South Asia, including both in India and in Nepal, menstruation is considered an impurity, and women experiencing it are quarantined from daily life, especially religious rituals.
“Women are more prone to snakebite during menstruation and pregnancy. Due to the belief that women should not sleep indoors or on beds during menstruation, they are forced to sleep in courtyards, cattle sheds and makeshift huts making them more vulnerable,” Dr. Acharya said.
Floods an issue, but not snakebite
Herpetologist and International Union for the Conservation of Nature (IUCN) specialist group member Kamal Devkota feels the government, besides reiterating the WHO target for reducing snakebites by 2030, has no clear policies or programs on reducing the harm from snakebites, other than to continue to provide anti-venom for free.
“It seems the loss of life and property from floods is increasing every year. But the problem of snakebites in Nepal is listed as a neglected health issue. Snakebite issues are not a priority for the Nepal government or donor agencies either,” he said.